(Note: Some of the links in this post are affiliate links, and we will be compensated when you make a purchase by clicking through our links at no additional cost to you.)
Finding Freedom: The Most Effective Treatments for Incontinence
Dealing with incontinence can be a challenging and sometimes embarrassing issue. But rest assured, you’re not alone in your journey. Millions of people worldwide experience incontinence, and there are effective treatments available to help you regain control of your life. In this comprehensive guide, we will explore the most effective treatment options for incontinence. From lifestyle changes and pelvic floor physical therapy, and proven online programs to medical interventions, we’ve got you covered. We’ll also provide valuable tips on managing the condition day-to-day. By the end of this article, you’ll have a better understanding of how to address incontinence and take steps toward a happier, more comfortable life.
Table of Contents
Understanding Incontinence
Incontinence is a condition characterized by the involuntary loss of urine or feces. It can affect people of all ages and genders, although it’s more common among women and older adults. The key to effective treatment lies in understanding the type of incontinence you’re dealing with and the underlying causes.
Types of Incontinence
- Stress Incontinence: This type of incontinence occurs when physical stress or pressure on the bladder causes leakage. Common triggers include sneezing, laughing, coughing, or heavy lifting.
- Urge Incontinence: Urge incontinence involves a sudden and intense urge to urinate, often resulting in leakage before reaching the bathroom. It can be caused by overactive bladder muscles or nerve problems.
- Mixed Incontinence: As the name suggests, mixed incontinence combines elements of both stress and urge incontinence. Individuals with mixed incontinence may experience leakage during physical activity and also struggle with sudden urges.
- Overflow Incontinence: This occurs when the bladder doesn’t empty completely, leading to frequent dribbling or leakage. It can be caused by an obstructed urinary tract or weak bladder muscles.
- Functional Incontinence: Functional incontinence is typically not due to bladder or pelvic issues but rather arises from physical or cognitive limitations that prevent an individual from reaching the bathroom in time.
Now that we’ve covered the different types of incontinence, let’s delve into various treatment options.
5 Effective Treatment Options For Incontinence:
Lifestyle Changes for Managing Incontinence
Before exploring medical interventions, consider making some lifestyle adjustments that can significantly improve your incontinence symptoms:
- Dietary Changes: Certain foods and drinks can irritate the bladder, including caffeine, alcohol, citrus fruits, and spicy foods. Reducing your consumption of these items can help alleviate symptoms.
- Hydration: While it may seem counterintuitive, drinking enough water is crucial to prevent concentrated urine, which can irritate the bladder. Aim for six to eight glasses of water a day.
- Weight Management: If you’re overweight, losing excess pounds can reduce pressure on the bladder and improve symptoms, especially in cases of stress incontinence.
- Regular Exercise: Engaging in low-impact exercises, such as walking and swimming, can help maintain a healthy weight and strengthen your pelvic floor muscles.
- Bladder Training: This involves gradually increasing the time between bathroom visits to help improve bladder control. It can be particularly effective for urge incontinence.
- Quit Smoking: Smoking can irritate the bladder and worsen incontinence symptoms. Quitting smoking can lead to significant improvements in bladder health.
While these lifestyle changes can be beneficial, they may not provide complete relief for everyone. That’s where specialized treatments come into play.
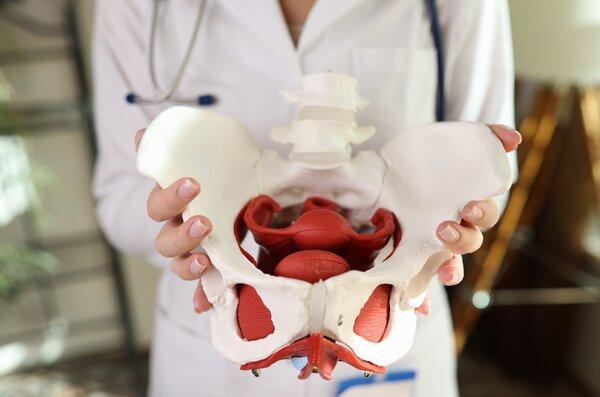
Pelvic Floor Physical Therapy: A Game-Changer
Pelvic floor physical therapy is a highly effective treatment option for many individuals dealing with incontinence. It involves working with a trained therapist who can assess your specific condition and develop a personalized treatment plan. Here’s why pelvic floor physical therapy is often a game-changer:
- Targeted Exercises: Pelvic floor physical therapists teach exercises that specifically target the muscles responsible for bladder and bowel control. These exercises, can strengthen weakened muscles or relax tensed muscles.
- Biofeedback: Some therapists use biofeedback techniques to help you understand and control your pelvic muscles better. This can be especially helpful for those who struggle to perform exercises correctly.
- Manual Therapy: Therapists may also use manual techniques to release tension in the pelvic floor muscles. This can improve muscle function and alleviate pain or discomfort.
- Education: Pelvic floor physical therapists educate patients about their condition, teaching them how to recognize triggers, manage symptoms, and make lifestyle changes that support bladder health.
- Postpartum Recovery: For new mothers, pelvic floor physical therapy can be essential in recovering after childbirth and addressing postpartum incontinence.
It’s important to note that pelvic floor physical therapy requires commitment and consistency. Results may not be immediate, but with time and effort, many individuals experience significant improvements in their incontinence symptoms.

Image Credit: flickr
Online Programs for Incontinence
In today’s digital age, a range of online programs offers effective incontinence treatment options, allowing you to comfortably pursue these programs from the convenience of your own home. Two notable programs in this domain are the MUTUsystem and Every-Mother:
MUTUsystem: This comprehensive online program focuses on pelvic health and recovery, providing exercises and educational content to address incontinence and diastasis recti.
Every-Mother: Tailored for mothers, this program emphasizes pelvic floor health, core strength, and overall well-being, helping women regain control post-pregnancy.
While Every-Mother.com is geared toward postpartum women, its exercises and principles can also benefit those experiencing incontinence due to pelvic floor weakness.
Medical Treatments
- Medications: Depending on the type of incontinence, your doctor may prescribe medications to relax the bladder or strengthen the urethral sphincter.
- Medical Devices: Some individuals benefit from devices like pessaries or urethral inserts.
- Botox Injections: Injections of botulinum toxin can relax an overactive bladder.
- Surgery: For individuals with severe incontinence or those who haven’t found relief with other treatments, surgical options may be considered, such as bladder sling surgery or artificial urinary sphincter placement. Surgery is typically reserved as a last resort when conservative treatments have proven ineffective.
Emotional and Psychological Support – Staying Positive
Incontinence can take an emotional toll, but maintaining a positive mindset is vital:
- Seek Support: Don’t hesitate to talk to friends, family, or a therapist about your feelings. Sharing your experiences can be cathartic and help you feel less isolated. Mental health professionals can also help you manage the emotional aspects of incontinence.
- Set Realistic Goals: Understand that managing incontinence is a journey. Set achievable goals and celebrate your successes, no matter how small they may seem.
- Stay Active: Engage in activities you enjoy and that make you feel good about yourself. Physical activity can boost your mood and overall well-being.
- Mindfulness and Relaxation: Consider practicing mindfulness, deep breathing, or meditation to reduce stress and anxiety, which can exacerbate incontinence.
Incontinence is a common condition, but it doesn’t have to control your life. With a better understanding of your type of incontinence and the available treatment options, you can take proactive steps toward regaining control and improving your quality of life. Remember, incontinence is a treatable condition.
Remember, you’re not alone in your journey to manage incontinence, and there are numerous resources and treatments available to help you lead a more comfortable and fulfilling life. Don’t hesitate to reach out to healthcare providers and specialists who can guide you toward the most suitable treatment plan for your unique needs. Take the first step toward freedom and take control of your life today.