(Note: Some of the links in this post are affiliate links, and we will be compensated when you make a purchase by clicking through our links at no additional cost to you.)
Understanding Stress Urinary Incontinence: Causes and Solutions
Stress urinary incontinence (SUI) is a common condition that affects millions of people, particularly women, around the world. It can be both physically and emotionally distressing, impacting one’s quality of life. If you or someone you know is dealing with SUI, it’s important to understand its main cause and explore potential solutions.
Table of Contents
What is Stress Urinary Incontinence (SUI)?
Stress Urinary Incontinence, often abbreviated as SUI, is a type of urinary incontinence that occurs when physical activities or movements put pressure on the bladder. This pressure can cause involuntary leakage of urine, which is both inconvenient and embarrassing. It’s called “stress” incontinence because it’s triggered by stress on the bladder rather than emotional stress.
The Main Cause of Stress Urinary Incontinence
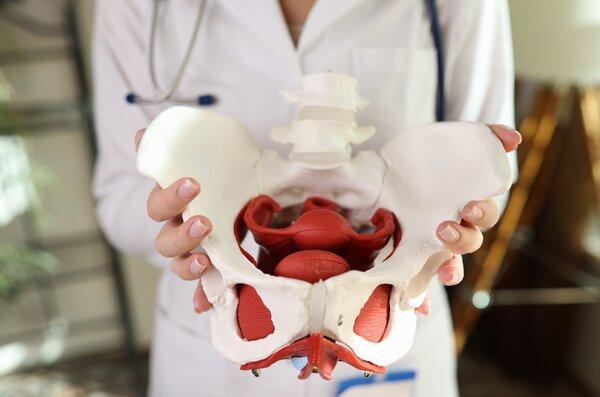
The primary cause of stress urinary incontinence is a weakening of the pelvic floor muscles and the urethral sphincter. These muscles play a crucial role in controlling the release of urine from the bladder. When they become weak or damaged, they are less effective at preventing urine leakage during moments of increased abdominal pressure.
The key factors contributing to the weakening of these muscles include:
Pregnancy and Childbirth:
- During pregnancy, hormonal changes and the pressure of the growing fetus can weaken pelvic floor muscles.
- Vaginal childbirth, especially if it involves forceps or vacuum extraction, can further stretch or damage these muscles.
Aging:
- As we age, our muscles naturally weaken, including those in the pelvic floor.
- This age-related muscle loss can lead to a higher risk of SUI in older individuals.
Hormonal Changes:
- Reduced estrogen levels, particularly during menopause, can contribute to muscle weakness in the pelvic region.
Obesity:
- Excess weight can put added pressure on the pelvic floor muscles and exacerbate SUI symptoms.
Chronic Coughing and Heavy Lifting:
- Activities that involve repeated heavy lifting or chronic coughing can strain the pelvic floor and lead to SUI.
Genetic Predisposition:
- Some individuals may have a genetic predisposition to weaker pelvic floor muscles, making them more susceptible to SUI.
Risk Factors for Developing SUI
While the main cause of SUI is weakened pelvic floor muscles, certain factors can increase your risk of developing this condition:
Gender:
- SUI is more common in women than in men. The female anatomy and the stresses of pregnancy and childbirth contribute to this gender disparity.
Age:
- As mentioned earlier, aging is a risk factor for SUI. The older you get, the higher the likelihood of muscle weakening.
Pregnancy and Childbirth:
- Women who have given birth, especially through vaginal delivery, are at a higher risk.
Obesity:
- Being overweight or obese increases the pressure on the pelvic floor, raising the risk of SUI.
Smoking:
- Smoking can lead to chronic coughing, which strains the pelvic floor muscles and may contribute to SUI.
Family History:
- If SUI runs in your family, genetics may play a role in your susceptibility.
Previous Pelvic Surgery:
- Surgeries in the pelvic area can damage or weaken the pelvic floor muscles, increasing the risk of SUI.
How to Diagnose SUI
If you suspect you have stress urinary incontinence, it’s important to seek a proper diagnosis from a healthcare professional. Your physician or pelvic floor physical therapist will perform a thorough evaluation, which may include:
a. Medical History: Your doctor will ask about your symptoms, medical history, and any relevant risk factors.
b. Physical Examination: A physical examination, including a pelvic exam, may be conducted to assess the strength and condition of your pelvic floor muscles.
c. Urinalysis: A urinalysis can help rule out other urinary tract issues that may be contributing to your symptoms.
d. Voiding Diary: Keeping a voiding diary, where you record when and how much you urinate, can provide valuable information about your condition.
e. Stress Test: A stress test involves activities like coughing or jumping to see if they trigger urine leakage.
f. Urodynamic Testing: In some cases, your physician may recommend urodynamic testing to assess how your bladder and urethra function.
Once diagnosed, you and your healthcare provider can discuss the most appropriate treatment options for managing your SUI.
>>> No More Leaks: Must-Read Urinary Incontinence Books
Lifestyle Changes to Manage SUI
In many cases, lifestyle modifications can significantly improve the symptoms of stress urinary incontinence. Here are some strategies to consider:
Pelvic Floor Exercises:
- Pelvic floor exercises involve contracting and relaxing the pelvic floor muscles to strengthen them.
- Regular, consistent pelvic floor exercises can improve muscle tone and reduce SUI symptoms.
Weight Management:
- Losing excess weight can alleviate pressure on the pelvic floor and reduce urine leakage.
Dietary Changes:
- Avoiding bladder irritants like caffeine, alcohol, and acidic foods can help reduce urgency and frequency of urination.
Fluid Management:
- Adjusting your fluid intake, especially in the hours leading up to bedtime, can minimize nighttime urinary incontinence.
Bladder Training:
- Gradually increasing the time between bathroom trips can help retrain your bladder and improve control.
Smoking Cessation:
- Quitting smoking can reduce chronic coughing and improve overall bladder health.
Medical Treatments for SUI
When lifestyle changes alone aren’t sufficient, medical treatments can be effective in managing SUI. Some options include:
Medications:
- Your doctor may prescribe medications that help strengthen the urethral sphincter or reduce bladder contractions.
Vaginal Devices:
- Pessaries are devices inserted into the vagina to support the bladder and reduce leakage.
Physical Therapy:
- Pelvic floor physical therapy involves working with a specialized therapist to strengthen and coordinate pelvic muscles.
Injections:
- Bulking agents can be injected into the tissue around the urethra to provide support and reduce leakage.
Surgical Options for SUI
- For individuals with severe or persistent SUI, surgical interventions may be necessary. Some surgical options include:
- Midurethral Sling Surgery – A sling is placed under the urethra to provide support and reduce leakage.
- Bladder Neck Suspension – This procedure involves lifting and supporting the bladder neck and urethra.
- Artificial Urinary Sphincter (AUS) – A small device is surgically implanted around the urethra to control the flow of urine.
- Botox Injections – In some cases, Botox injections into the bladder can relax overactive muscles and improve SUI symptoms.
- Collagen Injections – Collagen can be injected into the tissues around the urethra to provide support.
Taking Control of SUI
Suffering from stress urinary incontinence can be challenging, but it’s important to remember that you’re not alone, and there are various treatment options available. Lifestyle changes, such as weight management and pelvic floor exercises, can make a significant difference in managing your symptoms.
Moreover, online programs like MUTU System and Every-Mother can be great options for individuals looking to take control of their SUI. These programs offer convenient, at-home solutions that guide you through exercises and techniques specifically designed to strengthen your pelvic floor muscles and improve bladder control. They provide a supportive community and expert guidance, making it easier to stay motivated and track your progress.
While the main cause of stress urinary incontinence is the weakening of pelvic floor muscles, there are many effective ways to manage and treat this condition. Seek professional medical advice to determine the best approach for your individual needs. Whether it’s through lifestyle changes, medical treatments, or surgical interventions, taking action against SUI can greatly improve your quality of life and help you regain control over your bladder function. Remember, there is hope and help available to address stress urinary incontinence, allowing you to live life to the fullest.