(Note: Some of the links in this post are affiliate links, and we will be compensated when you make a purchase by clicking through our links at no additional cost to you.)
Exploring the Four Types of Urinary Incontinence: Understanding and Managing Your Condition
Urinary incontinence is a topic that affects millions of people worldwide, yet it often remains hidden behind a veil of embarrassment and stigma. If you’re experiencing urinary incontinence, please know that you’re not alone. In fact, understanding the different types of urinary incontinence can help you find the right solutions and regain control of your life.
In this post, we’ll delve into the four primary types of urinary incontinence, shedding light on what each one entails and offering practical advice for managing them. Whether you’re a sufferer seeking information or someone looking to support a loved one, this article aims to provide you with the knowledge and empathy you need.
Here are the four primary types of urinary incontinence:
1) Stress Incontinence
Stress incontinence is the most common type of urinary incontinence, affecting millions of women and men of all ages. This condition is characterized by the unintentional leakage of urine during physical activities that put pressure on the bladder, such as coughing, sneezing, laughing, or lifting heavy objects. So, what causes this frustrating condition?
Causes of Stress Incontinence
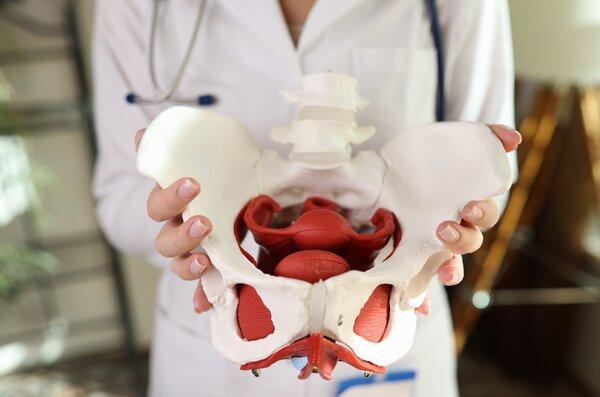
Stress incontinence primarily occurs due to weakened pelvic floor muscles. These muscles play a crucial role in supporting your bladder and urethra, helping to keep urine in check. Various factors can contribute to this weakening:
- Childbirth: The stress placed on the pelvic floor during childbirth can damage or stretch the muscles, leading to stress incontinence in some cases.
- Age: As we age, our muscles naturally weaken, including those in the pelvic region. This can result in stress incontinence, especially in older adults.
- Obesity: Carrying excess weight can increase pressure on the bladder and weaken the pelvic floor muscles, making stress incontinence more likely.
Managing Stress Incontinence
The good news is that stress incontinence is treatable and manageable. Here are some strategies to consider:
- Pelvic floor exercises: Strengthening the pelvic floor muscles through exercises like Kegel can significantly reduce or eliminate symptoms.
- Lifestyle changes: Losing weight, quitting smoking, and avoiding excessive caffeine and alcohol consumption can help improve symptoms.
- Pelvic floor physical therapy: This specialized form of physical therapy focuses on strengthening the pelvic floor muscles and improving bladder control. It can be highly effective in managing stress incontinence.
- Online programs: There are online programs like “Every Mother” and “Mutu System” designed to help individuals strengthen their pelvic floor muscles from the comfort of their own homes. These programs offer guided exercises and support, making them a convenient option for many.
- Medical interventions: In some cases, medical treatments like medications, vaginal pessaries, or surgery may be recommended.
2) Urge Incontinence
Urge incontinence, often referred to as overactive bladder (OAB), is another prevalent form of urinary incontinence. This condition is characterized by a sudden and intense urge to urinate, followed by involuntary leakage. People with urge incontinence may find themselves rushing to the restroom frequently, even waking up multiple times at night to urinate. But what triggers this uncontrollable urge?
Causes of Urge Incontinence
Several factors can contribute to urge incontinence:
- Neurological issues: Conditions like multiple sclerosis or stroke can disrupt the communication between the brain and the bladder, leading to an overactive bladder.
- Bladder irritants: Certain foods, beverages, and medications can irritate the bladder and trigger urges, including caffeine, spicy foods, and diuretics.
- Infection: Urinary tract infections (UTIs) can cause irritation and increase the frequency of urination.
Managing Urge Incontinence
Managing urge incontinence often involves a combination of lifestyle changes and medical interventions:
- Behavioral therapies: Techniques like bladder training, where you gradually increase the time between bathroom visits, can help regain control over your bladder.
- Pelvic floor exercises: These exercises can improve bladder control and reduce symptoms.
- Pelvic floor physical therapy: This specialized form of physical therapy highly beneficial for individuals experiencing urge incontinence. Through specialized exercises and techniques, this therapy helps strengthen the pelvic floor muscles, improving their ability to control bladder urges. By working with a trained pelvic floor physical therapist, patients can learn strategies to regain control over their bladder function, reduce the frequency of sudden urges, and ultimately enhance their quality of life.
- Online programs: Consider trying online programs like “Every Mother” and “Mutu System” to complement your treatment plan for urge incontinence. These programs offer structured exercises that can help strengthen the pelvic floor and improve bladder control.
- Medications: Your healthcare provider may prescribe medications to relax the bladder muscles or reduce irritation.
- Injections: In some cases, Botox injections into the bladder can help reduce urgency and frequency.

3) Overflow Incontinence
Overflow incontinence is a less common but equally challenging form of urinary incontinence. This condition occurs when the bladder doesn’t empty properly, leading to constant dribbling or leakage. It often makes you feel like your bladder is never fully empty, and it’s often associated with weak bladder muscles or an obstruction.
Causes of Overflow Incontinence
Several underlying factors can contribute to this type of incontinence:
- Blockage: An enlarged prostate in men, bladder stones, or tumors can obstruct the urethra and disrupt the normal flow of urine.
- Neurological issues: Conditions like diabetes or spinal cord injuries can interfere with the signals that control bladder function.
- Medications: Some medications, especially those used to treat high blood pressure or overactive bladder, can lead to overflow incontinence as a side effect.
Managing Overflow Incontinence
The treatment approach for overflow incontinence depends on the underlying cause:
- Catheterization: For severe cases, intermittent catheterization may be necessary to empty the bladder regularly.
- Medication adjustments: Your healthcare provider may need to modify your medication regimen to alleviate symptoms.
- Surgery: Surgical intervention may be required to remove obstructions or correct structural issues.
- Online programs: While online programs like “Every Mother” and “Mutu System” primarily focus on pelvic floor strengthening, they can still be beneficial in improving overall bladder function and reducing leakage associated with overflow incontinence.
- Pelvic floor physical therapy: A pelvic floor physical therapist can provide valuable assistance to individuals dealing with overflow incontinence. By targeting the pelvic floor muscles, pelvic floor physical therapy aims to enhance their strength and coordination, which can be particularly beneficial for those with weakened or impaired muscles contributing to the condition. Through tailored exercises and guidance, patients can improve their bladder function, reduce constant dribbling, and enhance their overall bladder control, thereby reducing the challenges associated with overflow incontinence.
4) Functional Incontinence
Functional incontinence is unique among the types of urinary incontinence as it is primarily associated with physical or cognitive impairments that hinder a person’s ability to reach the restroom in time. It’s not directly related to problems with the bladder or urinary tract.
Causes of Functional Incontinence
Functional incontinence can result from various conditions, including:
- Mobility issues: Arthritis, paralysis, or other mobility-limiting conditions can make it difficult to reach the bathroom quickly.
- Cognitive impairments: Conditions like dementia or Alzheimer’s disease can affect memory and awareness, making it challenging to recognize the need to urinate.
- Environmental factors: In some cases, the lack of accessible restrooms in public places or care facilities can contribute to functional incontinence.
Managing Functional Incontinence
Managing functional incontinence often involves addressing the underlying causes and implementing practical solutions:
- Mobility aids: Using mobility aids like walkers or wheelchairs can improve accessibility to the bathroom.
- Scheduled toileting: Establishing a regular bathroom schedule can help individuals with cognitive impairments.
- Environmental modifications: Ensuring easy access to restrooms in home and care facilities can be crucial.
- Online programs: While functional incontinence may not be directly related to pelvic floor muscle weakness, the online programs mentioned earlier can help individuals with physical impairments maintain their overall strength and mobility, potentially reducing the risk of accidents.
- Pelvic floor physical therapy: A pelvic floor physical therapist can offer significant support to individuals coping with functional incontinence. While this type of incontinence isn’t directly related to muscle weakness, these therapists can help patients improve their mobility and overall physical function. By addressing any underlying mobility or cognitive impairments and offering guidance on accessible restroom strategies, they empower individuals to navigate their daily lives more comfortably and with greater independence, ultimately reducing the impact of functional incontinence on their quality of life.
Urinary incontinence is a common and often treatable condition that can affect anyone, regardless of age or gender. Understanding the four primary types of urinary incontinence—stress, urge, overflow, and functional—is the first step toward effective management and improved quality of life.
If you or a loved one is struggling with urinary incontinence, don’t hesitate to seek help from a healthcare professional like a pelvic floor physical therapist. There are numerous treatment options available, ranging from lifestyle changes and exercises to medications, surgical interventions, and online programs like “Every Mother” and “Mutu System.” These programs can be a valuable addition to your journey toward regaining control and living life to the fullest. Remember, you’re not alone in this journey, and with the right support and information, you can regain control and live life to the fullest.